1. Silvestri KD, Carlotti AE. Subperiosteal implant : serving the dental profession for over 50 years. R I Dent J. 1995;28(1):11‑23.
2. Sconzo J. The complete mandibular subperiosteal implant : an overview of its evolution. J Oral Implantol. 1998;14‑5.
3. Schou S, Pallesen L, Hjorting-Hansen E, Pedersen C, Fibaek B. A 41-year history of a mandibular subperiosteal implant. Clin Oral Implants Res. 2000;(11):171‑8.
4. Bodine R, Yanase R, Bodine A. Forty years of experience with subperiosteal implant in 41 edentulous patients. J Prosthet Dent. janv 1996;75(1):33‑44.
5. Nguyen TM, Caruhel JB, Khonsari RH. A subperiosteal maxillary implant causing severe osteolysis. J Stomatol Oral Maxillofac Surg. déc 2018;119(6):523‑5.
6. Van Steenberghe D, Branemark PI, Quirynen M, De Mars G, Naert I. The rehabilitation of oral defects by osseointegrated implants. J Clin Periodontol. 1991;18(6):198‑205.
7. Nefussi JR. Le volume osseux résiduel après extraction dentaire est-il prédictible ? In: Mise en place chirurgicale et gestion des tissus muqueux péri-implantaires. p. 102‑21.
8. Nefussi JR. Biologie et physiologie du volume osseux implantable. In: EMC. Elsevier Masson SAS. Paris; 2011. p. 1‑12. (Medecine buccale; vol. 28).
9. Hienz SA, Paliwal S, Ivanovski S. Mechanisms of Bone Resorption in Periodontitis. J Immunol Res. 2015;2015:1‑10.
10. Cawood J, Howell R. A classification of the endetulous jaws. Int J Oral Maxillofac Surg. 1988;(17):232‑6.
11. Pietrokovski J, Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967;21‑7.
12. Urban IA, Nargusky H, Lozada JL. Horizontal ridge augmentation with a resorbable membrane and particulated autogenous bone with or without anorganic bovine bone-drived mineral : a prospective case series in 22 patients. Int J Oral Maxillofac Implants. avr 2011;26(2):404‑14.
13. Guillaume B. Accroissement osseux préimplantaire par disjonction osseuse. Inf Dent. 2004;86(1640).
14. Khoury F, Hanser T. Three-dimensional vertical alveolar ridge augmentation in the posterior maxilla : a 10-year clinical study. Int J Oral Maxillofac Implants. avr 2019;34(2):471‑80.
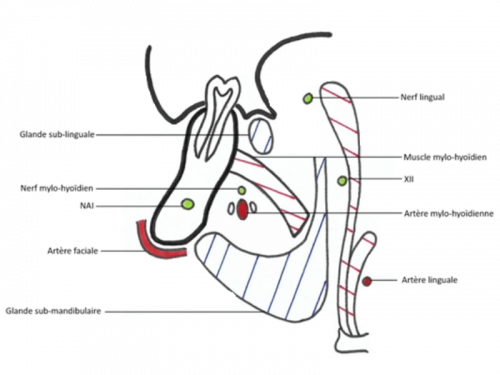
15. Laurentjoye M, Ella B, Caix P. La tête. In: Anatomie tête et cou. 2015e éd. Bordeaux: Bergeret; 2015. p. 3‑101.
16. Coutant JC, Martin R, Huault L, Ella B. Chirurgie du lambeau lingual. Inf Dent. 24 avr 2019;(16/17):35‑40.
17. Minichetti J. Analysis of HA-coated subperiosteal implants. J Oral Implantol.2003;29(3):111-6.
18. Cohen DJ, Cheng A, Kahn A, Aviram M, Whitehead AJ, Hyzy SL, et al. Novel Osteogenic Ti-6Al-4V Device For Restoration Of Dental Function In Patients With Large Bone Deficiencies: Design, Development And Implementation. Sci Rep. avr 2016;6(1):20493.
19. Claffey N, Bashara H, O’Reilly P, Polyzois I. Evaluation of New Bone Formation and Osseointegration Around Subperiosteal Titanium Implants with Histometry and Nanoindentation. Int J Oral Maxillofac Implants. sept 2015;30(5):1004-10.
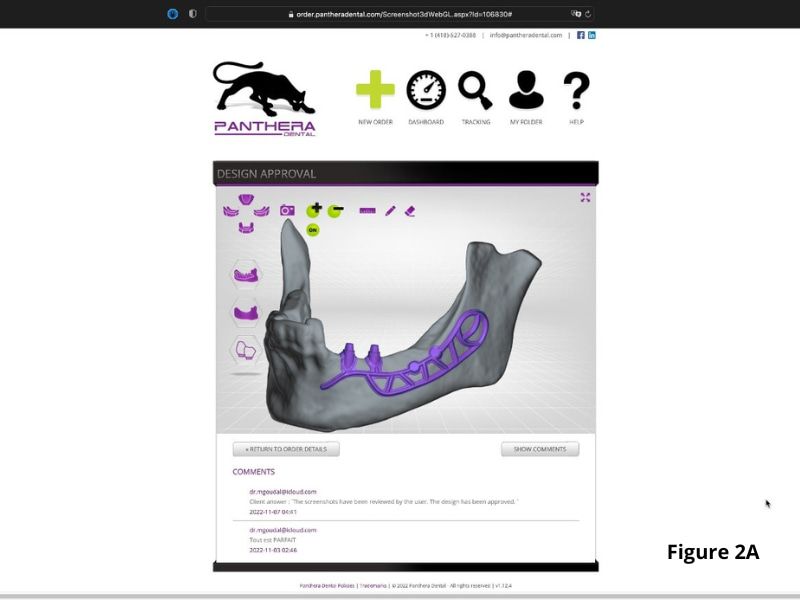
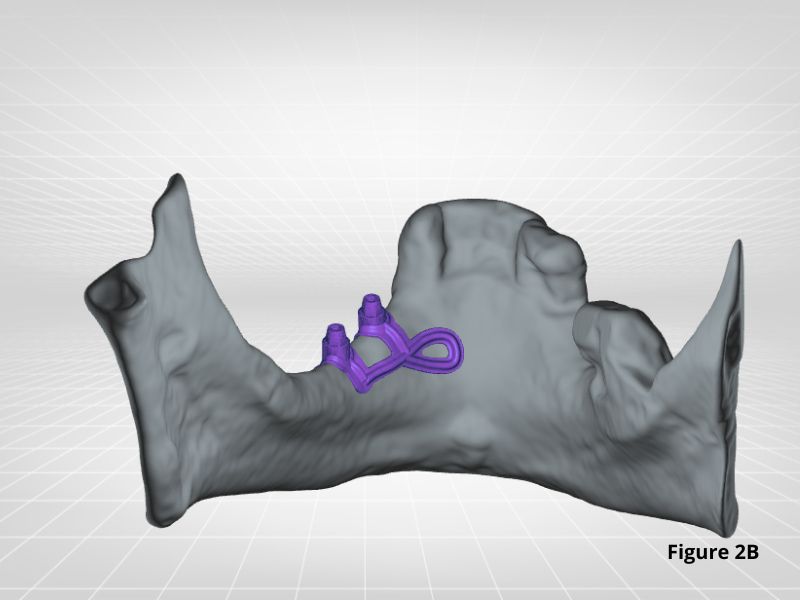
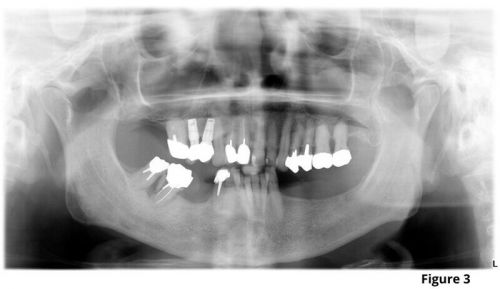
20. Cerea M, Dolcini G. Custom-Made Direct Metal Laser Sintering Titanium Subperiosteal Implants: A Retrospective Clinical Study on 70 Patients. BioMed Res Int. 28 mai 2018;2018:1‑11.
21. Mangano C, Bianchi A, Mangano F, Dana J, Colombo M, Solop I, et al. Custom-made 3D printed subperiosteal titanium implants for the prosthetic restoration of the atrophic posterior mandible of elderly patients: a case series. 3D Print Med. déc 2020;6(1):1.
22. Cohen DJ, Cheng A, Kahn A, Aviram M, Whitehead AJ, Hyzy SL, et al. Novel Osteogenic Ti-6Al-4V Device For Restoration Of Dental Function In Patients With Large Bone Deficiencies: Design, Development And Implementation. Sci Rep. avr 2016;6(1):20493.
23. Oren D, Dror AA, Bramnik T, Sela E, Granot I, Srouji S. The power of three-dimensional printing technology in functional restoration of rare maxillomandibular deformity due to genetic disorder: a case report. J Med Case Reports. déc 2021;15(1):197.
24. Gellrich NC, Zimmerer RM, Spalthoff S, Jehn P, Pott PC, Rana M, et al. A customised digitally engineered solution for fixed dental rehabilitation in severe bone deficiency: A new innovative line extension in implant dentistry. J Cranio-Maxillofac Surg. oct 2017;45(10):1632‑8.
25. Bolle C, Felice P, Barausse C, Pistilli V, Trullenque-Eriksson A, Esposito M. 4 mm long vs longer implants in augmented bone in posterior atrophic jaws: 1-year post-loading results from a multicentre randomised controlled trial. Eur J Oral Implant. 2018;11(1):31‑47.
26. Esposito M, Cannizzaro G, Soardi E, Pellegrino G, Pistilli R, Felice P. A 3-year post-loading report of a randomised controlled trial on the rehabilitation of posterior atrophic mandibles: short implants or longer implants in vertically augmented bone? Eur J Oral Implant. 2011;4(4):301‑3011.
27. Felice P, Barausse C, Pistilli R, Ippolito DR, Esposito M. Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Int J Oral Implant. 2019;12(1):25‑37.
28. Felice P, Pistilli R, Barausse C, Piattelli M, Buti J, Esposito M. Posterior atrophic jaws rehabilitated with prostheses supported by 6-mm-long 4-mm-wide implants or by longer implants in augmented bone. Five-year post-loading results from a within-person randomised controlled trial. Int J Oral Implant. 2019;12(1):57‑72.
29. Esposito M, Barausse C, Pistilli R, Piattelli M, Simone SD, Ippolito DR, et al. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Five-year results from a randomised controlled trial. Int J Oral Implant. 2019;12(1):39‑54.
30. Esposito M, Pellegrino G, Pistilli R, Felice P. Rehabilitation of posterior atrophic edentulous jaws: prostheses supported by 5 mm short implants or by longer implants in augmented bone? One-year results from a pilot randomised clinical trial. Eur J Oral Implant. 2011;4(1):21‑30.
31. Felice P, Pellegrino G, Checchi L, Pistilli R, Esposito M. Vertical augmentation with interpositional blocks of anorganic bovine bone vs. 7-mm-long implants in posterior mandibles: 1-year results of a randomized clinical trial: Vertical augmentation vs. 7-mm-long implants. Clin Oral Implants Res. déc 2010;21(12):1394‑403.
32. Felice P, Marchetti C, Iezzi G, Piattelli A, Worthington H, Pellegrino G, et al. Vertical ridge augmentation of the atrophic posterior mandible with interpositional bloc grafts: bone from the iliac crest vs. bovine anorganic bone. Clinical and histological results up to one year after loading from a randomized-controlled clinical trial. Clin Oral Implants Res. déc 2009;20(12):1386‑93.
33. Brandtner C, Borumandi F, Krenkel C, Gaggl A. A New Technique for Sandwich Osteoplasty with Interpositional Bone Grafts for Fixation. Int J Oral Maxillofac Implants. 19 sept 2014;29(5):1164‑9.
34. Geng Y, Zhou M, Parvini P, Scarlat S, Naujokat H, Abraha SM, et al. Sandwich osteotomy in atrophic mandibles: A retrospective study with a 2‐ to 144‐month follow‐up. Clin Oral Implants Res. oct 2019;30(10):1027‑37.
35. Marconcini S, Covani U, Giammarinaro E, Velasco-Ortega E, De Santis D, Alfonsi F, et al. Clinical Success of Dental Implants Placed in Posterior Mandible Augmented With Interpositional Block Graft: 3-Year Results From a Prospective Cohort Clinical Study. J Oral Maxillofac Surg. févr 2019;77(2):289‑98.
36. Felice P, Pistilli R, Lizio G, Pellegrino G, Nisii A, Marchetti C. Inlay versus Onlay Iliac Bone Grafting in Atrophic Posterior Mandible: A Prospective Controlled Clinical Trial for the Comparison of Two Techniques. Clin Implant Dent Relat Res. oct 2009;11:69‑82.
37. Laviv A, Jensen OT, Tarazi E, Casap N. Alveolar Sandwich Osteotomy in Resorbed Alveolar Ridge for Dental Implants: A 4-Year Prospective Study. J Oral Maxillofac Surg. févr 2014;72(2):292‑303.
38. Bianchi A, Felice P, Lizio G, Marchetti C. Alveolar distraction osteogenesis versus inlay bone grafting in posterior mandibular atrophy: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology. mars 2008;105(3):282‑92.
39. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. Interventions for replacing missing teeth: horizontal and vertical bone augmentation techniques for dental implant treatment. In: Cochrane Database of Systematic Reviews. 2009. (Issue 4).
40. Starch-Jensen T, Nielsen HB. Sandwich osteotomy of the atrophic posterior mandible with interpositional autogenous bone block graft compared with bone substitute material: a systematic review and meta-analysis. Br J Oral Maxillofac Surg. déc 2020;58(10):e237‑47.
41. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. The Efficacy of Horizontal and Vertical Bone Augmentation Procedures for Dental Implants: A Cochrane Systematic Review. Chiappelli F, éditeur. Eur J Oral Implant. 2009;2(3):167‑84.
42. Jensen OT. Alveolar Segmental “Sandwich” Osteotomies for Posterior Edentulous Mandibular Sites for Dental Implants. J Oral Maxillofac Surg. mars 2006;64(3):471‑5.
43. Pelo S, Boniello R, Moro A, Gasparini G, Amoroso PF. Augmentation of the atrophic edentulous mandible by a bilateral two-step osteotomy with autogenous bone graft to place osseointegrated dental implants. Int J Oral Maxillofac Surg. mars 2010;39(3):227‑34.
44. Marchetti C, Stefano T, Corinaldesi G, Felice P. Interpositional bone graft. Int J Periodontics Restorative Dent. 2007;27(6):547‑55.
45. Sohn DS, Shin HI, Ahn MR, Lee JS. Piezoelectric Vertical Bone Augmentation Using the Sandwich Technique in an Atrophic Mandible and Histomorphometric Analysis of Mineral Allografts: A Case Report Series. Restorative Dent. 2009;30(4):11.
46. Felice P, Iezzi G, Lizio G, Piattelli A, Marchetti C. Reconstruction of Atrophied Posterior Mandible With Inlay Technique and Mandibular Ramus Block Graft for Implant Prosthetic Rehabilitation. J Oral Maxillofac Surg. févr 2009;67(2):372‑80.
47. Felice P, Piana L, Checchi L, Corvino V, Nannmark U, Piattelli M. Vertical Ridge Augmentation of an Atrophic Posterior Mandible with an Inlay Technique and Cancellous Equine Bone Block : A Case Report. Int J Periodontics Restorative Dent. 2013;33(2):159‑66.
48. Roccuzzo A, Marchese S, Worsaae N, Jensen SS. The sandwich osteotomy technique to treat vertical alveolar bone defects prior to implant placement: a systematic review. Clin Oral Investig. mars 2020;24(3):1073‑89.
49. Elnayef B, Monje A, Albiol G, Galindo-Moreno P, Wang HL, Hernández-Alfaro F. Vertical Ridge Augmentation in the Atrophic Mandible: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. mars 2017;32(2):291‑312.