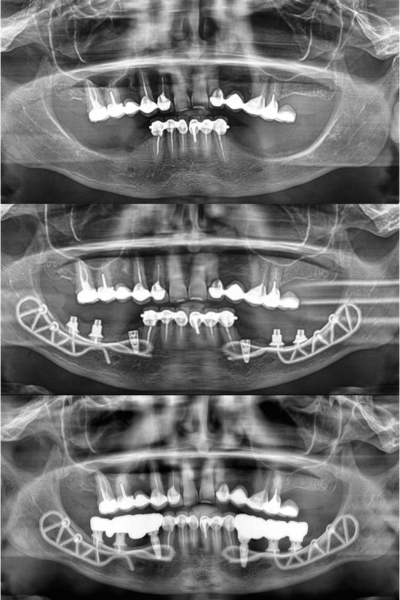
Subperiosteal implants for the rehabilitation of atrophic posterior mandibular regions
To this day, the dental implant rehabilitation of atrophic mandibular lateral regions remains a biological, temporal, and financial challenge. Thanks to CAD/CAM, titanium subperiosteal implants have become a viable alternative to conventional axial implants and bone regeneration.
Introduction
Subperiosteal implants, more recently called AMSJI (Additively Manufactured Subperiosteal Jaw Implants) by some authors(1), are an innovative concept in custom CAD/CAM implants. They perfectly match the ridge anatomy of patients with insufficient bone volume to receive endosteal implants traditionally used in axial implantology.
Dr. Gustave Dahl first described the concept of subperiosteal implants in 1940. However, the first implants, made of cobalt-chromium and using a direct bone impression from wide flap surgery, were not very successful. Their poor fit, lack of stability, and inability to osseointegrate resulted in an excessively high failure and complication rate.
With the advent of digital tools, it is now possible to perfect implant design using materials such as titanium. This advancement considerably improves fitting accuracy. As a result, subperiosteal implants have increased success rates and are becoming a relevant treatment option that deserves our attention.
Complexity of the posterior mandibular region
Treatment of atrophic posterior mandibular regions has long been a challenge in our rehabilitation procedures. The various treatment solutions depend on a number of parameters:
- Removable solutions are rarely accepted due to their initial bulkiness. Moreover, their instability leads to functional and aesthetic limitations. In the most severe cases, they can even cause pain when chewing due to the compression of the inferior alveolar nerve.(2)
- Implant solutions face several anatomical limitations. On one hand, there is a concomitant lack of height and width of the alveolar ridge, making vertical augmentation particularly difficult to achieve. On the other hand, the superficialization of the inferior alveolar nerve considerably increases the risk of postoperative nerve disorders. Finally, resorption of the bone surface leads to a reduction in the surrounding soft tissue, thus limiting the survival rate of the joint prosthesis.(3)
Various approaches have been developed to compensate for these numerous anatomical constraints:
- Several bone reconstruction techniques are used to restore sufficient crestal volume to allow the placement of endosteal implants. These methods include expansion, bone distraction, guided bone regeneration procedures using specific protocols such as the “sausage technique” or the use of titanium mesh, and bone blocks or mandibular framework.(4)(5)
- In direct contrast, basal implantology by definition consists of anchoring implants of specific design (disc, blade, plate, oblique, etc.) in the basal bone of the maxilla without the need for bone grafts.(6)
- Finally, subperiosteal implantology offers another treatment solution, as it requires neither bulky reconstruction nor bone anchorage. These implants are specially designed to adapt to residual bone and are positioned under the periosteum.
Planning and designing subperiosteal implants
After a patient with no contraindications to oral surgery is selected, Panthera implants are designed after collecting three pre-implant data:
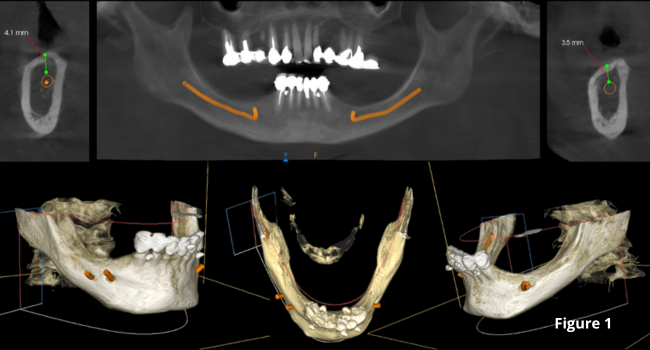
Figure 1: Initial CBCT examination (Carestream 9600)
- A Cone Beam exported in DICOM format. The success of the treatment depends largely on the accuracy and quality of the CT data. It is therefore advisable to opt for a large acquisition field, covering the entire mandible up to the posterior ascending ramus. In addition, the highest possible image resolution and the use of metal artifact reduction tools (such as the “MAR” – Metal Artefact Reductor) are essential to ensure optimal implant adaptation.(Figure 1)(7)
- An optical impression of the dento-mucosal surfaces.
- This is all combined with a digital wax-up, a preview of the future prosthetic project which will be exported in STL or PLY format. In the case of a limited number of residual teeth, radiopaque markers can be used to help combine the three data. (Figure 2) (8)(9)
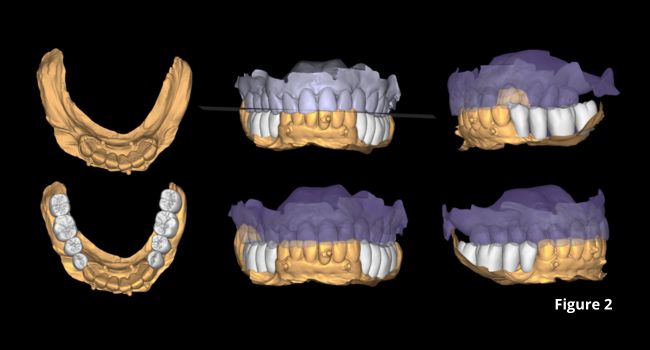
Figure 2: Optical impression (Primescan – Densply Sirona) and prosthetic project based on the antagonist arch (Design4me)
Dicom and STL files are transferred to the Panthera online platform. Once the order has been placed, a viewer allows you to follow and validate the implant creation stages. (Figure 3)
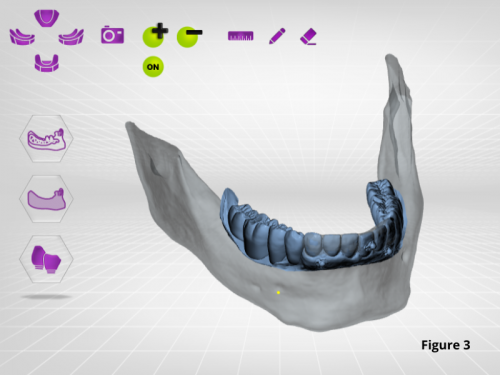
Figure 3: CBCT, optical impression, and digital wax-up uploaded to the Panthera platform dashboard
Implant modelling is performed by the company’s designers using their proprietary software, adapting to the clinical case and respecting a common structure. At the vestibular level, the exoskeleton bypasses the chin foramen, while osteosynthesis screws positioned more posteriorly stabilize the implant on the cortex of the external oblique line. A loop extends and completes the structure on the lateral surface of the ascending branch. Lingually, the framework forms a loop in the retro-symphyseal region and stops at the most distally located abutment, remaining coronal to the mylohyoid line. (Figure 4)
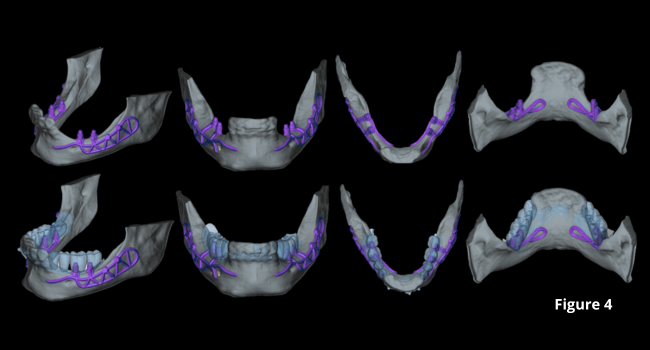
Figure 4:Subperiosteal implant design on the Panthera Dental platform. (Vestibular, frontal, occlusal, and lingual views)
Thanks to the evolution of materials, the development of digital tools, and the improvement of production techniques, Panthera is able to manufacture subperiosteal implants in grade 23 6AL 4V ELI titanium discs using 5-axis milling machines with a precision of 5 m. Finally, the surface finish is sandblasted in areas in contact with bone and the periosteum to promote bone regeneration.(10)(11)
Implants are supplied with a 3D resin model of the jaw. This model is used to check that implants fit perfectly before they are inserted. It also helps the operator find the ideal insertion axis, which should be achieved by distal translation followed by mesio-lingual rotation. This movement may differ slightly from one patient to another. (Figure 5)
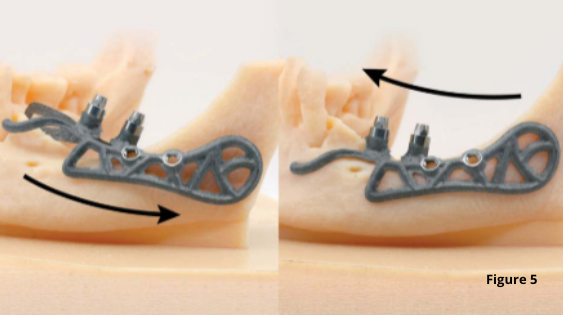
Figure 5: Ideal insertion axis for Panthera implants created on the 3D model
Surgical protocol
The procedure is performed under local anaesthetic and lasts between one and one-and-a-half hours per side. The first step is to raise a flap wide enough to allow adequate access to the surgical site. The crestal incision is made so as to evenly distribute the attached gingiva on either side of the future abutments. It extends to the anterior teeth via an intrasulcular incision and ends along the anterior edge of the ascending ramus.
The aim is to create full-thickness flaps to expose the chin foramen and protect the inferior alveolar pedicle on the vestibular side. The detachment should then continue beyond the external oblique line to the basal margin of the mandible, then to the insertion of the buccinator muscle without detaching it.
On the lingual side, it is also important to push back the sublingual compartment by lifting, still in full thickness, to the medial oblique line posteriorly and apically up to the anterior digastric fossa, avoiding effraction of the mylohyoid muscle and mental spines. (Figures 6 and 7)
(12)
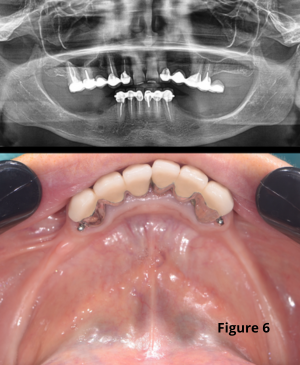
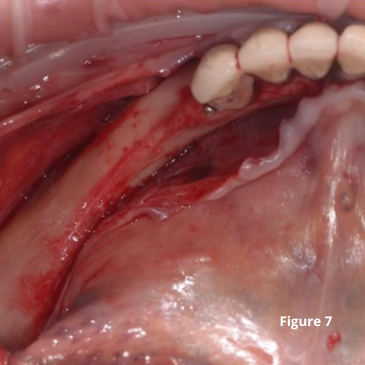
Figure 6: Pre-operative situation, panoramic radiograph and intra-oral photo / Figure 7: Incisions and flap detachment
Some clinicians may choose to use a technique for one-piece subperiosteal implants. However, the author notes that one-piece bilateral subperiosteal implants are more difficult to insert, making surgery more complex. The surgery time while the flaps are detached is longer with a one-piece bilateral subperiosteal implant, increasing the risk of complications, infections, pain, edema, and discomfort for the patient. If there are minor or major complications, it’s easier to manage them when there are two unilateral subs. Finally, thanks to the large bone/implant contact surface, there is great stability even with a unilateral sub implant, making no difference between a bilateral or two unilateral.
Before inserting the implants, a “soft brushing” technique can be used to relax the flaps and thus allow tension-free closure of the site while preserving the periosteum. The bone is then scraped to ensure that any residual fibrous tissue is removed.
The implant is inserted along the recommended axis, validated beforehand on the resin model. It is advisable to leave the healing abutments in place and use hemostatic forceps to facilitate gripping of the implant, while remaining clear of the subgingival portion during the placement procedure. (Figures 8, 9 and 10)
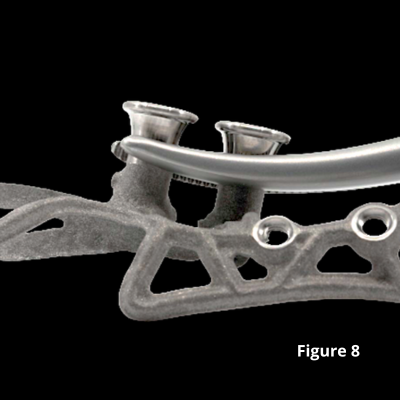
Figure 8: The Panthera SUB implant is gripped to facilitate insertion without damaging it
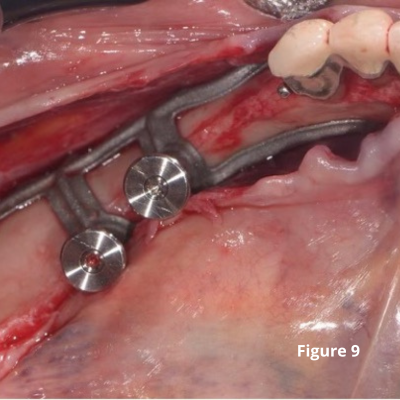
Figure 9: Positioning the implant and checking its fit (occlusal view)
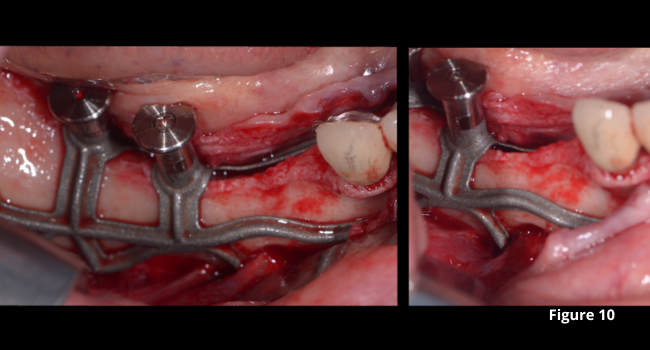
Figure 10: Positioning the implant, checking its fit, and highlighting the chin foramen (vestibular view)
Once the position and fit have been carefully checked, the implant is stabilized using two osteosynthesis screws. A drilling guide is also provided to facilitate the procedure. (Figure 11)


Figure 11A, 11B: Drilling guide and implant retaining screws
In this specific case, two endosteal implants are placed simultaneously in positions 34 and 44. PRF membranes are positioned to optimize gingival healing. (Figure 12) Finally, the flaps are sutured tension-free using apical and crestal mattress stitches.

Figure 12: Covering implants with PRF membranes
Prosthetic steps
After four months of osseointegration, the second surgical stage will uncover the buried implants, and a 15-day gingival maturation period around the healing abutments will be observed before proceeding with the prosthetic steps. (Figure 13)

Figure 13: Second surgical stage after four months of osseointegration and placement of healing abutments
Transgingival abutments for subperiosteal implants are similar to those used for endosseous implants. These are tapered abutments designed for a fixed, screw-retained prosthesis. The steps involved in using prostheses are the same as for conventional techniques:
- Physical impression using the pick-up technique (Figure 14);
- Fitting mock-ups to validate the prosthetic project (Figure 15);
- Final screwing of permanent prostheses (Figure 16).

Figure 14: Physical impression

Figure 15: Fitting mock-up

Figure 16: Permanent prostheses screwed in
Conclusion
The rehabilitation of atrophic postero-mandibular areas is a major surgical challenge. In certain clinical situations, the limits of implant and bone reconstruction therapies may be reached. Thanks to the evolution of CAD/CAM technologies and the improved accuracy of CBCTs, the subperiosteal technique is becoming a genuine treatment alternative. Thanks to their unique surgery with no bone contribution, subperiosteal implants are a minimally invasive approach. Post-operative recovery and the risk of complications are thus reduced. Healing times prior to prosthetic rehabilitation are also reduced for the patient. First developed over 80 years ago, this solution is now more sophisticated and biocompatible than its historical counterpart, with reliable and promising results.